Many wide complex tachycardias originate in the ventricles, but not all. The ones that don't include a bundle branch block, and a ventricular reentry problem, where the ventricles contract too early after a partial repolarization – like a pre-excited tachycardia or Wolff-Parkinson-White (WPW) syndrome.
In this lesson, we'll look at monomorphic ventricular tachycardia (including an ECG), polymorphic ventricular tachycardia, or (thankfully) PVT for short (also including an ECG), and pulseless ventricular tachycardia. And at the end of the lesson, we'll provide a Word about treatments based on the type of tachycardia.
Monomorphic Ventricular Tachycardia
One very common V-tach is called monomorphic ventricular tachycardia, which means that all of the complexes are the same size, direction, and shape. It's usually caused by an ectopic pacemaker located somewhere in the ventricles.
An ECG for a patient with monomorphic V-tach will exhibit the following signs.
*Monomorphic V-tach ECG for Pediatric Patient
| 1. |
Rhythm |
regular, but could also be slightly irregular |
| 2. |
Rate |
between 100 and 200 beats per minute |
| 3. |
P-waves |
rarely discernible |
| 4. |
PR interval |
not discernible |
| 5. |
QRS complex |
greater than .11 seconds, wide and strange-looking |
| 6. |
P:QRS ratio |
does not exist |
The main problem with this type of fast and wide complex tachycardias is that the hemodynamics are unstable. The heart rate is so fast that it inhibits the atrium from prefilling and preloading the ventricles before the next contraction. In these cases, it's important to know whether or not the patient is stable or unstable.
Pro Tip #1: If the patient is stable, try to learn more about why the patient could be experiencing this type of arrhythmia. And remember, wide complex V-tach can sometimes be caused by heart disease, electrolyte imbalance (especially potassium) and a Q to T interval prolongation.
If the patient is stable, check to see if their rhythm is supraventricular or ventricular in origin.
Warning: If the patient is unstable, immediate treatment is vital.
Polymorphic Ventricular Tachycardia
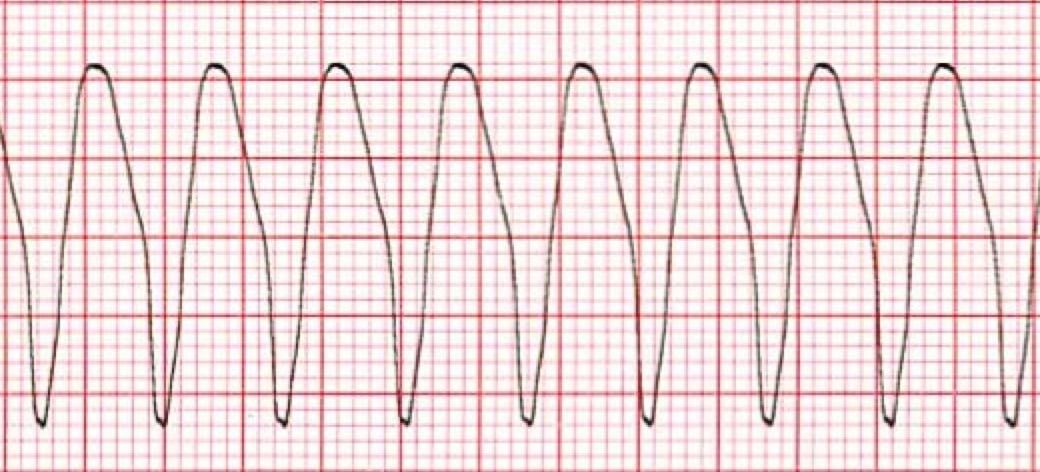
Poly simply means multiple and describes the origin of electrical foci in the ventricles. In fact, polymorphic V-tach is caused by multiple ventricular foci with the resulting QRS complexes varying in axis, amplitude, and duration.
Polymorphic V-tach can also be described as bi-directional V-tach, which is another type of polymorphic V-tach that is commonly associated with digoxin toxicity, commonly known as torsades de pointes.
Along with digoxin toxicity, we often see polymorphic V-tach with hypokalemia or hypomagnesemia.
An ECG for a patient with polymorphic V-tach will exhibit the following signs.

* Polymorphic Ventricular Tachycardia ECG for Pediatric Patient
| 1. |
Rhythm |
irregular |
| 2. |
Rate |
between 200 and 250 beats per minute |
| 3. |
P-waves |
not discernible |
| 4. |
PR interval |
missing |
| 5. |
QRS complex |
variable, but greater than .11 seconds, wide and strange |
| 6. |
P:QRS ratio |
missing |
In torsades, it can sometimes appear that the apex of the V-wave changes from top to bottom and back again. And actually, torsades (French in origin) literally translates as a twisting of points.
The most important thing to remember with this type, along with monomorphic wide-complex V-tach, is that both can become pulseless V-tach or VFib pretty quickly.
Pulseless Ventricular Tachycardia
Pro Tip #2: One important thing to remember is that wide complex V-tach can present with or without a pulse and you may even see pulseless V-tach in a cardiac arrest patient. However, in most cases, pulseless V-tach will quickly deteriorate into VFib.
Also keep in mind that pulseless V-tach is treated the same as VFib and that recognition of the condition and treatment for it will be vital for a potential positive outcome.
Pro Tip #3: An ECG interpretation for pulseless V-tach can be the same for pulsed V-tach. The difference is that the patient is unresponsive, not breathing normally, and has no pulse.
A Word About Treatments Based on Type of Tachycardia
Distinguish between supraventricular and ventricular rhythms can be difficult. Most wide complex tachycardias are ventricular in origin, particularly if the patient is older or has underlying heart disease.
If the patient is pulseless, you should treat the rhythm as VFib and follow the cardiac arrest algorithm.
If the patient has a wide complex tachycardia and is also unstable, you should assume it's V-tach until proven wrong. The amount of energy required for cardioversion of V-tach is determined by the following morphologic characteristics.
1. If the patient is unstable but has a pulse with regular, uniform wide complex V-tach, or monomorphic V-tach:
- Treat with synchronized cardioversion and an initial shock of 100 joules
- If there is no response to the first shock, it's reasonable to increase the dose in a stepwise fashion
2. Arrhythmias with a polymorphic QRS appearance, or polymorphic V-tach, such as torsades de pointes, will usually not permit synchronization. If the patient has polymorphic V-tach:
- Treat as VFib with high-energy, unsynchronized shocks, such as defibrillation doses
If there is any doubt about whether an unstable patient has monomorphic or polymorphic V-tach, don't delay treatment for further rhythm analysis. Instead, go right into providing high-energy, unsynchronized shocks.