Table of Contents
- What Is CPR?
- What Is a Defibrillator?
- When Is a Defibrillator Needed?
- How Can I Learn CPR & Defibrillation?
- Defibrillation FAQs
You’ve likely seen an automated external defibrillator (AED) used in your favorite medical drama, or maybe you’ve spotted one hanging on the wall of the restaurant you frequent. But have you ever wondered, “What is a defibrillator?” and would you know how to use one in the face of an emergency?
While education and awareness of life-saving protocols like CPR and AED use have helped bring their existence to the mainstream public, many people don’t actually know what, exactly, a defibrillator is. Further, many are unaware of the impact an AED can have when paired with proper CPR techniques.
Read on to learn the answers to “What is a defibrillator?,” “How does a defibrillator work?,” and “How can CPR and a defibrillator help save a life?”
What Is CPR?
CPR stands for cardiopulmonary resuscitation and is used to help treat sudden cardiac arrest. This life-saving technique’s origins date back to 1956, when Peter Safar and James Elam first invented mouth-to-mouth resuscitation. CPR training programs were eventually developed in 1960 and quickly spread to share this intervention with physicians.
CPR consists of seven easy steps and two primary actions: chest compressions and rescue breaths. While both actions are essential to a person whose life is in danger, the process has changed over the years. Before 2010, the ABC (airway, breathing, compressions) approach was recommended; after 2010, new research suggested a CAB model was more effective.
The International Liaison Committee on Resuscitation (ILCOR) updates CPR guidelines every five years by researching and assessing new findings to ensure the current best practices are shared across the globe.
How Can CPR Save a Life?
CPR is effective because it helps maintain the life-sustaining roles that the heart and lungs perform in circulating oxygen-rich blood throughout the body until trained medical aid can step in.
When it comes to effectively administering CPR, chest compressions must be performed at the correct rate. Songs with between 100 and 120 beats per minute, like “Stayin’ Alive” by the Bee Gees or “Dancing Queen” by ABBA, can help you keep the right pace. In some cases, chest compressions may suffice. In most others, you may need to find the nearest AED.
So now that you know what CPR is and why it’s so important to help save a life, what is a defibrillator, and how does it work in conjunction with CPR?
Benefits of Early CPR & Defibrillation
When it comes to saving lives during sudden cardiac arrest, the faster you act, the better the chances of the victim recovering. Early CPR combined with defibrillation significantly increases the chances of survival by restoring blood flow and resetting the heart’s normal rhythm.
Here’s why acting fast is so important:
- It improves survival rates. CPR keeps the blood flowing while defibrillation helps reset the heart. Together, they can increase someone’s chance of survival by as much as 10-20 times, especially if done within the first few minutes.
- It protects the brain. Time matters when it comes to oxygen. Without it, brain cells start to die in just a few minutes. Jumping in with CPR and an AED can help protect someone from lasting brain damage.
- You don’t have to be a doctor. AEDs are designed for anyone to use — yes, even if you’ve never touched one before. The device will walk you through the steps, so you can feel confident stepping in to help.
- It buys precious time. Think of CPR and defibrillation as holding the fort until the professionals arrive. It keeps the person stable, giving them a better chance at recovery when the ambulance gets there.
- It empowers communities. Knowing how to use an AED and perform CPR means more people can step in and save a life. Schools, workplaces, gyms, or anywhere else people gather become safer places.
At the end of the day, it’s about being prepared to act.
With CPR and defibrillation, you don’t have to be a superhero or a certified medical professional to make a difference.
What Is a Defibrillator?
While the general public is aware that a defibrillator is a tool that shocks people in an emergency, they’re not especially clear on what’s really happening when they hear that popular phrase, “Clear!” So what is a defibrillator, exactly?
A defibrillator is a device that uses electricity to shock a person’s heart out of an abnormal rhythm and return it to a typical sinus rhythm. One of the most commonly available types of defibrillator is an AED, which can be found in public spaces. Look for a heart with a lightning bolt across, which signifies that the area has an AED storage space.
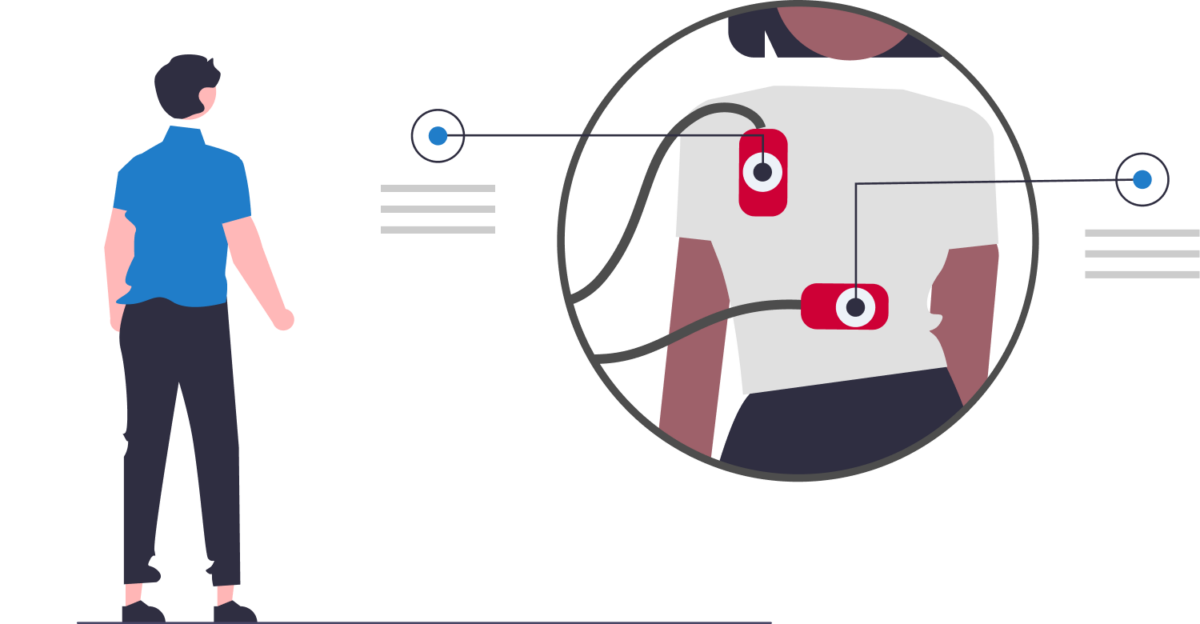
AEDs contain two electrical leads that connect the device to two sets of sticky patches as well as instructions for using the AED. Also, most 911 dispatchers can provide instruction through the phone, so call 911 when in doubt. The AED will automatically analyze the victim’s heart rhythm and provide appropriately timed shocks to return the heart to a normal rhythm.
Once you can answer “What is a defibrillator?” we recommend learning how to use one. In certain emergencies, knowing how to perform CPR and use an AED can increase a person’s chances of survival far more than performing CPR alone.
How Does a Defibrillator Work?
A defibrillator is a device designed to interrupt the chaotic electrical activity in the heart during cardiac arrest, harnessing the power of electrical energy in a way that’s both targeted and controlled.
In the first stage, the defibrillator detects the heart’s electrical signals to identify abnormal rhythms like ventricular fibrillation or ventricular tachycardia. These are life-threatening conditions where the heart quivers instead of pumping blood effectively.
In the second stage, the device analyzes the heart’s activity and will only act when it’s needed — typically with life-threatening arrhythmias like ventricular fibrillation (VF) or ventricular tachycardia (VT) to prevent unnecessary harm.
An AED will detect heart rhythms, analyze activity, and deliver a shock if one is needed based on the analysis.
If a shock is required, the third stage begins with the delivery of a precise burst of electrical energy. This energy travels through the chest, momentarily halting all electrical activity in the heart. By essentially “stunning” the heart, the chaotic signals are stopped, allowing the heart’s natural pacemaker to regain control.
The electrical shock works by briefly depolarizing the heart’s muscle cells. This disrupts the erratic signals causing cardiac arrest, pausing the heart’s activity so it can start fresh. The amount of energy delivered is carefully calibrated to ensure it’s strong enough to be effective but not so strong as to cause further damage.
After the shock, the heart may resume its normal rhythm, but CPR should be resumed regardless. This can help maintain blood flow while the device reassesses after 2 minutes and prepares to deliver another shock if necessary.

What Are the Different Types of Defibrillators?
While all defibrillators do the same general job in providing an electrical shock to a heart, each has its own best-use scenario. Here’s what to know about the three common types and when you might use each one.
- Automated external defibrillator (AED): AEDs are the most visible and publicly known types of defibrillators in use today. They’re used solely in emergency situations that arise suddenly and aren’t intended to be used by someone with long-term needs for fibrillation due to cardiac concerns.
These devices are specifically designed for public use, even by individuals with no medical training. AEDs analyze the heart’s rhythm automatically and determine whether a shock is necessary. They guide users through the entire process with clear voice instructions and visual prompts, ensuring anyone can step in and provide life-saving aid.
Their presence in schools, airports, gyms, and other public places has made them critical tools for responding to sudden cardiac arrests outside of medical settings.
- Implanted cardioverter defibrillator (ICD): ICDs may be suggested by a physician for patients who have a high risk of lethal heart arrhythmias that are likely to persist long-term. An ICD is a surgically implanted device used to provide electrical shocks when needed to reset the heart’s rhythm — unlike pacemakers, which are used to speed up a slow heart rate.
Once implanted, an ICD continuously monitors the heart’s electrical activity to detect life-threatening arrhythmias. If a dangerous rhythm is identified, the ICD delivers an automatic shock to correct it without any intervention required from the patient.
This real-time monitoring and rapid response capability make ICDs invaluable for individuals at high risk of sudden cardiac events.
- Wearable cardioverter defibrillator (WCD): Also known as a wearable external vest, a WCD is an alternative for those who aren’t eligible for a surgically implanted ICD. WCDs analyze a person’s heart rate to provide electrical shocks when needed and are relatively new to the market (they’ve only been FDA approved since 2002).
These devices offer a noninvasive option for patients who need temporary protection, such as those recovering from a cardiac event or awaiting a permanent ICD. Worn under clothing, WCDs provide constant monitoring and immediate intervention for safety during vulnerable periods. While not as discrete or permanent as ICDs, WCDs are a great option for patients in transition or with specific medical needs.
ICDs and WCDs are prescribed solely by medical professionals. Although AEDs need a prescription to be purchased, they are designed to be accessible to and used by the general public and are commonly used by both medical professionals and laypeople.
How Have Defibrillators Evolved Over Time?
Defibrillators have advanced significantly since their inception, evolving from bulky, hospital-bound devices to portable, user-friendly tools accessible to the public.
In the late 19th century, early experiments with electrical shocks laid the groundwork for defibrillation, but the first successful use on a human occurred in 1947 during open-chest surgery. These initial devices were invasive and cumbersome, limiting their use to hospitals.
By the 1960s, external defibrillators became more practical, allowing shocks to be delivered through electrodes on the chest. This era also saw the development of implantable cardioverter defibrillators (ICDs), which became viable for long-term use by the 1980s.
Introduced in the 1990s, AEDs were designed for layperson use with automated prompts and public placement, drastically improving out-of-hospital survival rates.
The early 2000s brought wearable cardioverter defibrillators (WCDs), offering noninvasive protection for patients at temporary cardiac risk. Modern defibrillators are now smaller, smarter, and more effective, featuring real-time feedback and integration with healthcare systems.
These innovations have made defibrillators indispensable in saving lives, both inside and outside medical settings.
What Are Some Common Defibrillator Concerns?
One of the most popular questions we get besides “What is a defibrillator?” is “Is this thing safe to use, or am I going to get shocked?”
While we agree that electricity should be always respected as electrical shock can be a very real risk to your health, there are very minimal risks to using an AED. These devices have been designed with specialty conductive gels and foam insulators that help prevent an AED’s electrical pulse from arcing from one person to another.
What Are Some Common Defibrillator Myths?
Beyond the most basic of defibrillator concerns, there are a lot of myths surrounding the question “What is a defibrillator?” as well as how they actually work to help save lives. Here are a few of the most prevalent ones:
- You have to rub the paddles together. People commonly assume that rubbing the paddles together builds a static charge to provide the needed “shocking power.” This concept came from manual heart monitors before the adhesive pads were FDA-approved. It is rare to find any medical professionals using paddles today. Modern AEDs use their own battery power pack to provide the appropriate amount of electrical shock once it has analyzed the victim’s heart rhythm.
- A defibrillator is meant to restart a stopped heart. We’ve all seen our favorite medical drama patient flatline and be revived by an electrical shock, but a defibrillator doesn’t restart a stopped heart. It can only correct an improper electrical signal being sent to the heart.
- A defibrillator will electrocute you if the victim is wet. While electricity and water certainly don’t mix, being wet doesn’t increase your or the victim’s risk of electrical shock due to the intelligent analysis that AEDs conduct before providing a shock. It’s more likely that the patches won’t stick well enough to give a reading. However, it’s still important to make sure the victim is not in a large puddle of water and ensure their chest is dry so the AED pads stick.
- If you have to ask, “What is a defibrillator?” you shouldn’t use one. We can certainly understand not wanting to hurt someone by using a tool you’re unfamiliar with, but the safety measures built into modern AEDs help keep victims and rescuers safe. Most AEDs also include step-by-step guides and picture directions.
- You can stop a healthy person’s heart if you use a defibrillator on them. As mentioned, one of the key steps in using an AED is the analysis of a person’s heart, which will be interpreted by the AED to only provide an electrical shock if appropriate. A healthy person would not need, and thus would not receive, a shock. When the AED is shocking a victim, ensure no one is touching the victim.
- You shouldn’t use an AED on a pregnant woman. While there are specific recommendations about providing effective CPR to a pregnant woman, pregnant women face no more of a risk than any other person experiencing a medical emergency. The baby’s best chance of survival is the mother’s survival.
The best cure for misinformation is always quality education, and being able to answer, “What is a defibrillator?” is just the first step in building your CPR knowledge. Although you can use an AED without proper training to save a life, we highly suggest that everyone be trained in first aid, CPR, and AED use in case of an emergency.
Who Should Own an Automated External Defibrillator?
Some public spaces are required by law not only to have an AED on site but also to ensure that there are personnel trained to use the device and that the device is easily identifiable (though rules vary by state, city, and even county). But aside from public spaces, who else might benefit from owning an AED?

If you or someone you live with has a family history of cardiac concerns, an AED might be good to have on hand in case of an emergency. As mentioned above, an AED is not a long-term stand-in where an ICD may be more appropriate, but if risk factors for needing resuscitation are present, it’s always best to be prepared.
Beyond the home, health-related professionals — such as first responders, security guards, and lifeguards — who are responsible for the public’s well-being could benefit from carrying an AED in the event that they need to step in to help in an emergency.
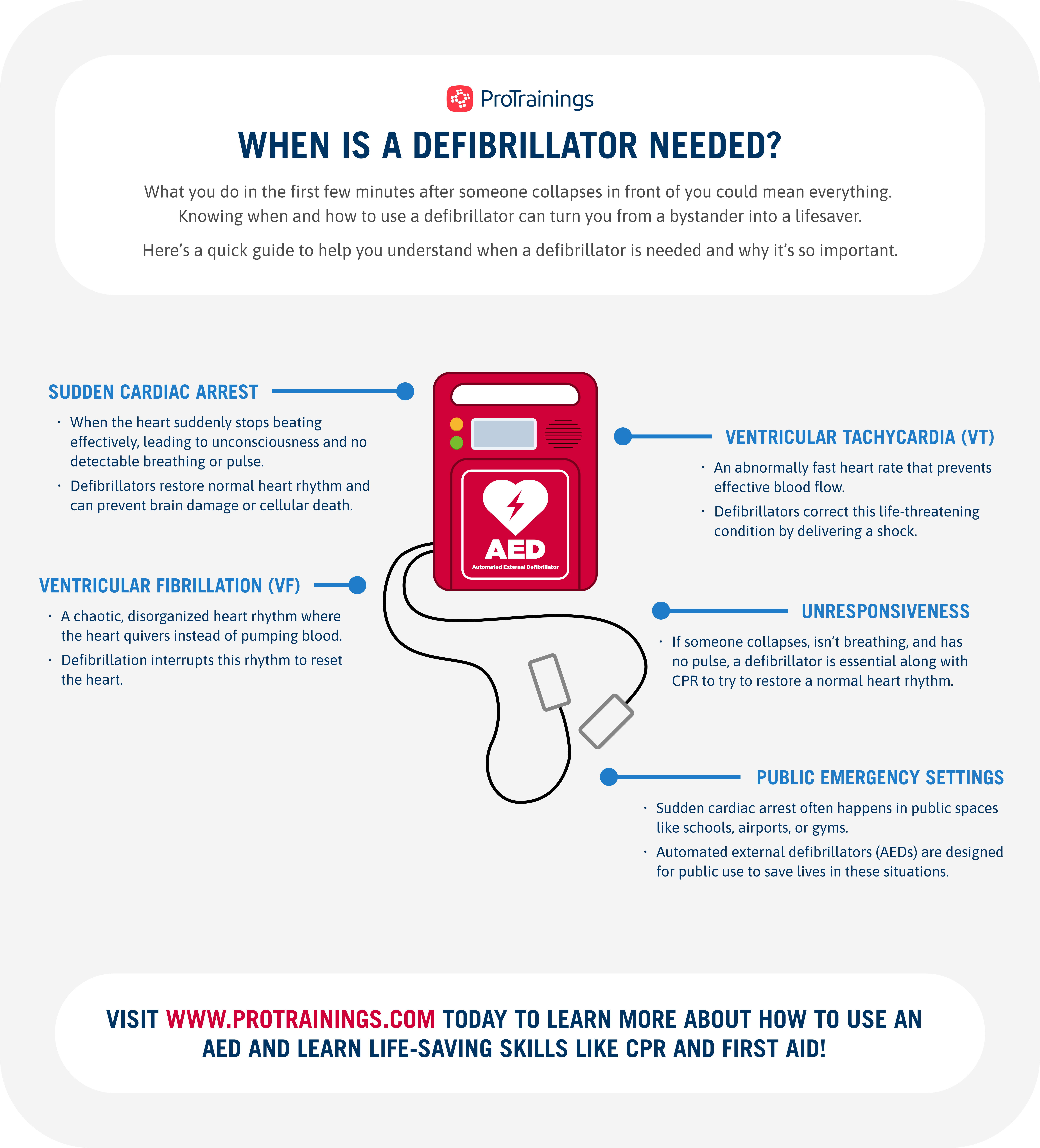
When Is a Defibrillator Needed?
A defibrillator is needed when the heart’s electrical system malfunctions, leading to life-threatening arrhythmias like ventricular fibrillation (VF) or ventricular tachycardia (VT). These conditions cause the heart to quiver ineffectively rather than pumping blood to the body and brain.
Defibrillators are commonly used in emergency situations, such as out-of-hospital cardiac arrests, or healthcare settings when a patient’s condition rapidly deteriorates. Other cardiac interventions like cardioversion and pacemakers address different heart rhythm issues and situations, highlighting the versatility of modern cardiac care.
How Is Cardioversion Different From Defibrillation?
Cardioversion and defibrillation both involve delivering electrical shocks to the heart, but they serve different purposes and are used in distinct circumstances.
Cardioversion is typically planned and used to treat less severe arrhythmias, such as atrial fibrillation (AFib) or atrial flutter. It is synchronized with the heart’s electrical cycle to restore a normal rhythm in a controlled setting, often with sedation for patient comfort.
In contrast, defibrillation is an emergency procedure used during sudden cardiac arrest caused by life-threatening arrhythmias like VF or VT. The shock is delivered immediately, without synchronization, to stop chaotic electrical activity in the heart.
While cardioversion aims to fine-tune the heart’s rhythm, defibrillation is a lifesaving measure designed to restart it entirely.
How Is a Pacemaker Different From Defibrillation?
Pacemakers and defibrillators both address heart rhythm problems but in very different ways.
A pacemaker is a small, surgically implanted device that continuously monitors and regulates the heart’s rhythm by delivering gentle electrical pulses to speed up a heart that is beating too slowly (bradycardia). It’s a long-term solution that works in real time to maintain a steady heartbeat.
Defibrillation, on the other hand, involves a stronger electrical shock to stop dangerously fast or chaotic rhythms like VF or VT. It is used in emergencies to reset the heart’s electrical system, not to maintain a regular rhythm over time. While pacemakers act as a preventative measure, defibrillators are a reactive tool for immediate intervention during cardiac arrest.
How Can I Learn CPR & Defibrillation?
Through our experienced team of instructors, our students are able to learn more about how to properly combine CPR and AED interventions. Our certification courses that cover CPR and AEDs take a look at the considerations behind when to use an AED and how to properly integrate it into effectively providing CPR — but nothing can replace quality training.
Many people avoid taking the step to seek out CPR and AED training because they think the training is going to be expensive, boring, or difficult to fit into their busy schedules. Depending on your lifestyle, remote learning online may be worth looking into for your CPR and AED training.
Not only does online training help bring quality education to you, but also the bite-sized videos can be reviewed at your own pace so you can retain the knowledge you’d need in an emergency. Whether recertification is a requirement for your career or you want to buff up your résumé for a job opportunity, our online training is a perfect option.
We believe that knowing the answers to “What is a defibrillator?” and “How do you perform CPR?” is half the battle. The confidence that comes with certifying your skills is the other half. Understanding how a defibrillator works can mean the difference between life and death, empowering you to act decisively in critical moments.
Through public awareness and broader accessibility to these lifesaving devices, we can create safer communities where everyone is prepared to step in during emergencies.
Defibrillation FAQs
Defibrillators are critical tools for saving lives during cardiac emergencies, but many people have questions about their safety, use, and effectiveness. Below, we answer some of the most common questions about defibrillators.
- Is a defibrillator safe to use?
Yes, defibrillators are designed with safety in mind. Automated external defibrillators (AEDs) include built-in safeguards to ensure that a shock is only delivered if necessary. Modern devices analyze the heart’s rhythm and prevent inappropriate shocks, making them safe for use by trained and untrained individuals alike. - Can an untrained person use a defibrillator?
Absolutely. AEDs are specifically designed for public use and include clear voice prompts and visual instructions to guide users step by step. While CPR and AED training are beneficial, untrained bystanders can still use AEDs effectively, as the device ensures that no harm is done if a shock is not required. - Can I use an AED on a child?
Yes, although there are some preferred settings for a child, an adult AED can be used on a child or infant. If your AED has pediatric pads or a child setting, be sure to use those as they provide the best treatment for children. In the limited data available, using adult pads does not cause harm but has an unnecessary potential risk. - Does a defibrillator restart the heart?
Not exactly. A defibrillator delivers an electrical shock to stop chaotic heart rhythms, allowing the heart’s natural pacemaker to reset and establish a normal rhythm. It’s a common misconception that a defibrillator “restarts” the heart; instead, it helps correct life-threatening arrhythmias. - What happens after using a defibrillator?
After defibrillation, the patient’s condition may stabilize, but continued CPR and immediate medical attention is still critical. Emergency responders will take over care, performing advanced medical interventions as needed. If the defibrillation is successful, the patient must still be transported to a hospital for further evaluation and treatment. - What is the recovery time after defibrillation?
Recovery time varies depending on the cardiac event. What caused the cardiac arrest and how long it took before the patient had a pulse again are two major factors in recovery time. Patients have rarely been known to wake up almost immediately, while others may take several days to wake up if they were placed in a medically induced coma. - How effective are defibrillators?
Defibrillators are highly effective in treating ventricular fibrillation and ventricular tachycardia, the most common causes of sudden cardiac arrest. When used promptly, they can greatly increase a person’s chances of survival, especially when combined with high-quality CPR.
What is the survival rate for defibrillation in cardiac arrest cases?
Survival rates vary based on how quickly defibrillation is administered. If used within the first few minutes of cardiac arrest, survival rates can be as high as 50-70%. This highlights the importance of immediate action and the widespread availability of AEDs.
What is the survival rate for defibrillation in cardiac arrest cases?
Survival rates vary based on how quickly defibrillation is administered. If used within the first few minutes of cardiac arrest, survival rates can be as high as 50-70%. This highlights the importance of immediate action and the widespread availability of AEDs.
ProTrainings’ experienced, knowledgeable staff can help to ensure that your staff is not only certified for administrative peace of mind but also prepared for every scenario. Contact us today to learn more about how ProTrainings can help you make getting your staff CPR certified easier and more efficient.